|
Getting your Trinity Audio player ready... |
Comprehensive Guidelines for Managing Prediabetes Updated: October 2025
Prediabetes is a metabolic condition where blood glucose levels are elevated beyond the normal range but are not yet high enough to qualify as type 2 diabetes. This intermediate state of glucose dysregulation places individuals at increased risk of progressing to diabetes, as well as developing cardiovascular complications. It affects roughly one-third of adults in the United States and an estimated 720 million people globally.
Many individuals with prediabetes are unaware of their condition because it usually presents without clear or noticeable symptoms. However, early identification and intervention can significantly reduce the risk of developing full-blown type 2 diabetes and other associated health issues.
Understanding and Identifying Prediabetes
Before a diagnosis of type 2 diabetes is made, most people pass through a phase of impaired glucose regulation, often referred to as prediabetes. During this phase, blood sugar levels are higher than what is considered normal but not yet within the diabetic range. While some people may begin to exhibit mild symptoms typical of diabetes—such as fatigue, increased thirst, or frequent urination—many do not show any signs at all.
Because prediabetes is largely asymptomatic, routine screening and risk assessment are crucial for early detection and prevention.
Diagnostic Criteria for Prediabetes
The criteria for diagnosing prediabetes vary slightly among major health organizations, including the American Diabetes Association (ADA), the World Health Organization (WHO), and the International Expert Committee. These criteria are based on different glucose measurements:
1. Impaired Fasting Glucose (IFG):
- Defined by a fasting blood glucose level between 100 to 125 mg/dL (5.6–6.9 mmol/L) according to ADA guidelines.
2. Impaired Glucose Tolerance (IGT):
- Measured during a 2-hour oral glucose tolerance test (OGTT) with 75 grams of glucose.
- IGT is diagnosed when the 2-hour post-load glucose value is between 140 to 199 mg/dL (7.8–11.0 mmol/L).
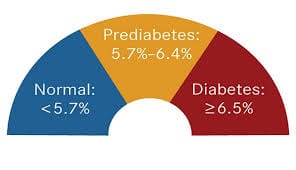
3. Hemoglobin A1c (HbA1c):
- ADA defines prediabetes as an HbA1c level between 5.7% and 6.4% (39–47 mmol/mol).
- The International Expert Committee defines it as 6.0% to 6.4%.
HbA1c has the advantage of being convenient, as it does not require fasting. However, its reliability can be affected by several health conditions such as anemia, iron deficiency, pregnancy, and kidney disease, which can influence red blood cell turnover and skew results.
Who Should Be Screened for Prediabetes or Diabetes?
The ADA has established clear guidelines for screening asymptomatic adults who may be at increased risk:
Testing is recommended for adults who:
- Have a BMI ≥25 kg/m² (or ≥23 kg/m² for Asian Americans) and possess at least one of the following risk factors:
- Family history of diabetes (first-degree relative)
- Belong to a high-risk ethnic group (African American, Latino, Native American, Asian American, Pacific Islander)
- History of cardiovascular disease
- Diagnosed hypertension (≥140/90 mmHg) or are on antihypertensive therapy
- Low HDL cholesterol (<35 mg/dL) and/or high triglyceride levels (>250 mg/dL)
- Women with polycystic ovary syndrome (PCOS)
- Sedentary lifestyle
- Presence of insulin resistance-related conditions such as severe obesity or acanthosis nigricans
Other testing recommendations:
- Individuals previously diagnosed with prediabetes (based on A1C, IFG, or IGT) should be screened annually.
- Women with a history of gestational diabetes should undergo lifetime screening every 3 years.
- For individuals with no identified risk factors, testing should begin at age 45.
- If test results are within the normal range, repeat testing at least every three years is advised.
- People living with HIV should also undergo screening for diabetes and prediabetes.
Managing Prediabetes: Prevention is Key
Prediabetes offers a critical window for intervention. Lifestyle changes, when implemented effectively, can significantly reduce the risk of progression to type 2 diabetes—by as much as 58%, according to landmark studies like the Diabetes Prevention Program (DPP).
a) Lifestyle Interventions
- Dietary Adjustments:
- Aim to reduce daily caloric intake by approximately 500–700 kcal.
- Focus on limiting saturated fats and refined sugars.
- Emphasize high-fiber, whole-food-based diets that include vegetables, fruits, lean proteins, and whole grains.
- Physical Activity:
- Engage in moderate-intensity physical activity (like brisk walking) for at least 30 minutes per day, 5 days a week or more.
- This equates to a minimum of 150 minutes per week.
- Weight Management:
- For those who are overweight or obese, the goal is typically a weight loss of at least 7% of total body weight.
- Even modest weight loss has been shown to significantly improve glucose regulation.
- Other Lifestyle Factors:
- Quit smoking, as it contributes to insulin resistance and cardiovascular disease risk.
- Improve sleep hygiene, aiming for 7–9 hours of quality sleep per night.
- Incorporate stress-reducing techniques like meditation, yoga, or counseling.
- Support and Monitoring:
- Start with frequent in-person follow-up visits, particularly in the early stages of lifestyle change.
- Later, this can be scaled back to less frequent check-ins, with the option for virtual consultations for convenience.
b) Pharmacological Therapy
If lifestyle modifications alone do not yield sufficient improvements in blood glucose levels—especially in individuals with multiple risk factors or who are unable to make significant lifestyle changes—metformin may be considered as a preventive therapy.
Metformin is especially recommended for:
- Individuals under age 60 with prediabetes and additional risk factors (e.g., obesity, family history of diabetes)
- Women with a history of gestational diabetes
- Those with a rising HbA1c despite lifestyle interventions
Monitoring considerations:
- Long-term metformin use has been associated with vitamin B12 deficiency, so patients on extended therapy should be regularly screened and supplemented as needed.
Conclusion
Prediabetes is a crucial warning sign that requires timely intervention. While it may not present immediate symptoms, the long-term risks associated with unmanaged blood sugar levels—such as progression to type 2 diabetes, cardiovascular disease, and nerve damage—are significant.
The good news is that early detection and proactive management—primarily through lifestyle adjustments, with medications when necessary—can prevent or delay the onset of diabetes and significantly improve long-term health outcomes. Routine screening, especially in high-risk populations, combined with personalized care plans, can help reverse or control prediabetes effectively.