|
Getting your Trinity Audio player ready... |
Understanding Methotrexate: Uses, Mechanisms, Interactions, and Dosing
Understanding Methotrexate is a widely used medication in clinical practice, primarily known for its effectiveness in treating autoimmune diseases, certain cancers, and even in medical abortion. Its diverse therapeutic applications, along with the potential risks it poses, make understanding how it works and how it is dosed crucial for both healthcare professionals and patients. In this article, we will explore the mechanisms behind methotrexate’s action, its interactions with other drugs, and why it is typically administered once weekly for certain conditions.
What Is Methotrexate?
Methotrexate is a type of disease-modifying antirheumatic drug (DMARD) that is most commonly used in the management of autoimmune diseases, including rheumatoid arthritis and severe psoriasis. It is also employed in chemotherapy regimens for treating various cancers, including leukemia, lymphoma, and some solid tumors such as breast cancer. Additionally, methotrexate is used as a medical intervention for abortions.
The dosage of methotrexate varies widely depending on the condition being treated. In the context of inflammatory conditions like rheumatoid arthritis or psoriasis, lower doses are used compared to the higher doses required for chemotherapy. The dosing regimen also involves adjusting the drug’s frequency to reduce the risk of side effects. For example, patients undergoing chemotherapy with methotrexate typically receive higher doses with more frequent administration, which is counterbalanced by rescue therapy to minimize toxicity.
Side Effects of Methotrexate
While methotrexate is highly effective, it does come with a range of potential side effects. Some common side effects associated with methotrexate include:
- Ulcerative stomatitis: Inflammation and ulcers in the mouth.
- Bone marrow suppression: Decreased production of blood cells, leading to anemia and increased risk of infection.
- Hair loss: A common side effect, especially in higher doses used for cancer treatment.
- Nausea and vomiting: Frequently reported, particularly when higher doses are administered.
- Hypersensitivity reactions: Allergic responses that can range from mild to severe.
- Hepatic cirrhosis: Long-term use of methotrexate can lead to liver damage.
- Pulmonary fibrosis: A rare but serious lung condition that can develop with prolonged methotrexate use.
Because of the significant risk of these side effects, monitoring of liver function and blood cell counts is crucial during methotrexate treatment.
How Does Methotrexate Work?
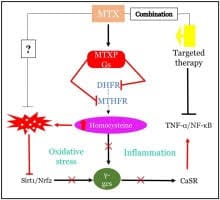
Methotrexate operates through two primary mechanisms: as an antimetabolite and as an immunosuppressant.
- Antimetabolite Action
As an antimetabolite, methotrexate inhibits the enzyme dihydrofolate reductase (DHFR), which is essential for converting dihydrofolate into tetrahydrofolate (THF). THF is a critical cofactor in the synthesis of nucleotides, which are building blocks for DNA and RNA. By disrupting the production of these nucleotides, methotrexate effectively inhibits DNA and RNA synthesis, making it especially useful in cancer treatments where rapidly dividing cells, like cancer cells, require constant DNA replication.
This inhibition also interferes with the production of proteins needed for cell division, which is why methotrexate is effective against cancers such as leukemia, lymphoma, and certain solid tumors. The reduction in DNA and RNA synthesis limits the growth of cancerous cells.
- Immunosuppressive Action
Methotrexate’s immunosuppressive effects are particularly valuable in treating autoimmune diseases like rheumatoid arthritis. In autoimmune conditions, the immune system mistakenly attacks healthy tissues, and methotrexate helps to reduce this hyperactive immune response. Methotrexate achieves this by inhibiting inflammatory cytokines such as interleukin-6 (IL-6), interleukin-8 (IL-8), and tumor necrosis factor-alpha (TNF-alpha), all of which are involved in the inflammatory process. By reducing the activity of these cytokines, methotrexate helps control inflammation and manage conditions like rheumatoid arthritis and psoriasis.
Drug Interactions with Methotrexate
Methotrexate interacts with a number of medications, and these interactions can significantly alter its effectiveness and increase the risk of adverse effects. Some notable interactions include:
- Penicillins and NSAIDs: Both of these drugs can decrease the renal clearance of methotrexate, increasing its concentration in the body and raising the risk of toxicity. This can lead to severe side effects, including liver damage and bone marrow suppression.
- Folate Antagonists: Drugs such as trimethoprim (an antibiotic) and phenytoin (an anticonvulsant) are folate antagonists like methotrexate. When used together, they can increase the risk of blood disorders, such as anemia or thrombocytopenia (low platelet count).
- Clozapine: An antipsychotic medication, clozapine has been associated with an increased risk of neutropenia (low neutrophil count) when combined with methotrexate. This can lead to severe infections, as neutrophils play a key role in fighting bacterial infections.
Because of these interactions, it is important for healthcare providers to monitor drug combinations closely and adjust dosages as necessary to avoid potential complications.
Why Is Methotrexate Taken Once Weekly?
The frequency of methotrexate administration depends on the condition being treated. For inflammatory conditions such as rheumatoid arthritis and severe psoriasis, methotrexate is often prescribed once a week. This dosing schedule is designed to minimize side effects while still providing effective treatment.
Rheumatoid Arthritis and Psoriasis
In the case of rheumatoid arthritis, the once-weekly dosing helps balance the drug’s effectiveness in reducing inflammation and slowing disease progression while minimizing the risk of toxicity. For psoriasis, methotrexate is typically prescribed as a divided dose taken over the course of one day, but it is still administered weekly.
Chemotherapy
When methotrexate is used in chemotherapy, the doses are much higher and are administered more frequently than in the treatment of inflammatory conditions. However, chemotherapy regimens often include rescue therapy with other medications, such as leucovorin, to reduce the risk of toxicity. This regimen differs significantly from the lower, less frequent doses given to patients with rheumatoid arthritis or psoriasis.
Risk of Toxicity
Taking methotrexate daily or at higher frequencies for extended periods can increase the risk of severe side effects, such as liver damage (hepatotoxicity), bone marrow suppression, and gastrointestinal distress. Therefore, the once-weekly dosing schedule for conditions like rheumatoid arthritis is designed to reduce these risks while still providing sufficient therapeutic benefit.
Why Is Folic Acid Taken with Methotrexate?
Folic acid is commonly prescribed alongside methotrexate, usually on a day other than the day the methotrexate dose is taken. The role of folic acid is to help mitigate some of the side effects associated with methotrexate, particularly those related to the gastrointestinal system, liver function, mouth sores, and anemia.
Folic acid does not interfere with the therapeutic effects of methotrexate in treating autoimmune conditions because the anti-inflammatory action of methotrexate is due to its suppression of certain cytokines, rather than its inhibition of folate metabolism. However, folic acid is avoided in cancer treatments with methotrexate because it could potentially counteract the drug’s ability to inhibit folate metabolism, which is crucial for its anticancer effects.
Conclusion
Methotrexate is a versatile and potent medication used to treat a variety of conditions, from autoimmune diseases like rheumatoid arthritis and psoriasis to cancers and medical abortions. Its ability to suppress immune activity and inhibit cell division through its antimetabolite effects makes it a cornerstone of many treatment regimens. However, the potential for severe side effects, particularly with long-term use, requires careful monitoring and appropriate dosing. The once-weekly dosing schedule for inflammatory conditions helps to minimize the risk of toxicity while still providing effective treatment, making methotrexate a valuable tool in the management of chronic diseases.