|
Getting your Trinity Audio player ready... |
Triptans Pharmacology: An In-Depth Review
Triptans are a class of medications primarily used in the treatment of acute migraine and cluster headaches. These drugs have become a mainstay in managing these conditions since their introduction in the early 1990s. While they are effective for symptomatic relief, they do not serve as preventive treatments and are not considered a cure. Triptans are classified as abortive agents, meaning that they work to alleviate the headache once it has started, rather than preventing future attacks. This article provides an extensive review of triptans’ pharmacology, including their indications, mechanism of action, side effects, and drug interactions.
Indications for Use:Triptans
Triptans are primarily indicated for the treatment of acute migraine attacks and cluster headaches. These are two distinct types of severe headache disorders, each with unique pathophysiology. For migraines, triptans are used once the headache has started, and the medication aims to shorten the duration of the attack and reduce associated symptoms such as nausea, vomiting, and sensitivity to light and sound. In cluster headaches, which are known for their extremely painful, one-sided headaches that occur in cyclical patterns, triptans provide rapid relief.
However, it is important to note that triptans are not used for the treatment of other types of headache, such as tension-type headaches, which are less severe and are not associated with the complex mechanisms involved in migraines or cluster headaches. Additionally, triptans are not prophylactic agents, meaning they do not prevent future migraine or cluster headache episodes. Rather, they are abortive medications, which means they help to end or alleviate an ongoing attack.
Since their development in the 1990s, triptans have largely replaced ergotamine derivatives, which were previously used to treat migraines but were less effective and had a higher incidence of side effects. The introduction of sumatriptan, the first triptan approved by the U.S. Food and Drug Administration (FDA) in 1993, marked a significant advancement in the acute management of migraines. Since then, several other triptans have been introduced, each offering its own advantages in terms of potency, onset of action, and side effect profile.
Mechanism of Action
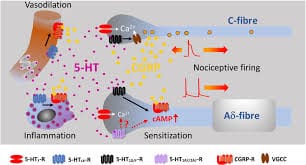
The pharmacological action of triptans revolves around their ability to act on specific serotonin receptors in the brain, known as 5-HT1B and 5-HT1D receptors. Serotonin (5-HT) is a neurotransmitter that plays a significant role in regulating mood, vascular tone, and pain perception. The connection between serotonin activity and migraine relief has been suspected for decades, dating back to research in the 1940s, but it was not until the 1990s that triptans became widely used as a treatment.
Triptans work primarily through the following mechanisms:
- Vasoconstriction: The activation of 5-HT1B receptors leads to the constriction of blood vessels around the brain. This is believed to counteract the vasodilation that occurs during a migraine attack. In a migraine, blood vessels in the brain dilate, contributing to the pain and discomfort. By constricting these blood vessels, triptans reduce the throbbing pain associated with migraines and cluster headaches.
- Inhibition of neuropeptide release: Triptans also inhibit the release of certain neuropeptides, particularly Substance P and CGRP (calcitonin gene-related peptide), which are involved in the transmission of pain signals. These neuropeptides are released from nerve terminals during a migraine attack and contribute to the inflammatory processes in the brain. By preventing their release, triptans help to mitigate the pain and associated symptoms of a migraine.
- Inhibition of nociceptive neurotransmission: Finally, triptans reduce the transmission of pain signals in the brainstem, particularly by acting on pain-processing pathways. This inhibition of nociceptive (pain-sensing) neurotransmission helps to dampen the overall perception of pain during a migraine or cluster headache.
Together, these three mechanisms enable triptans to effectively abort or reduce the severity of a headache once it has started.
Commonly Prescribed Triptans
Several triptans are available for the treatment of acute migraine and cluster headaches. These include:
- Sumatriptan: The first triptan to be approved by the FDA in 1993, sumatriptan remains one of the most widely prescribed triptans for both acute migraine and cluster headaches.
- Eletriptan: Known for its longer half-life and more potent effects, eletriptan is often used when patients experience inadequate relief with sumatriptan.
- Zolmitriptan: This triptan has both oral and nasal spray formulations, offering patients flexibility in how they take the medication during a migraine attack.
- Almotriptan: Almotriptan is similar to sumatriptan but is noted for having a lower incidence of side effects, making it a good option for patients with sensitivity to medications.
- Rizatriptan: Rizatriptan is known for its fast onset of action, and it is frequently used in patients who require rapid relief from migraine attacks.
While these drugs are effective, each triptan has its own pharmacokinetic properties, including half-life and bioavailability, which may affect the choice of therapy depending on the patient’s needs and preferences.
Side Effects
Triptans are generally well-tolerated, but like any medication, they are associated with potential side effects. Common side effects include:
- Paresthesias: A tingling or “pins and needles” sensation, often felt in the fingers or toes.
- Nausea: Some patients may experience gastrointestinal symptoms, including nausea, although this is typically mild and transient.
- Chest pain: Some patients report a sensation of chest tightness or pain, which can be concerning. Although rare, this side effect can sometimes be a sign of cardiovascular issues.
- Sweating: Some individuals may experience increased perspiration as a side effect.
- Muscle pain: Some people may report muscle aches or discomfort.
- Weakness: A general sense of fatigue or weakness may occur.
- Dry mouth: A common side effect in some individuals taking triptans.
While most of these side effects are mild, there is a small risk of more serious cardiovascular effects, including hypertension and coronary artery constriction, which is why triptans are contraindicated in patients with established cardiovascular disease. Sumatriptan, in particular, has been linked to sulfhemoglobinemia in cases of overdose. This rare condition causes blood to appear green due to a sulfur group being incorporated into the hemoglobin molecule. Fortunately, this condition is reversible once the medication is discontinued.
Drug Interactions
Triptans can interact with various other medications, increasing the risk of adverse effects or reducing the effectiveness of either drug. Notably, serotonin syndrome is a potential concern when triptans are taken in combination with SSRIs, SNRIs, MAO inhibitors, or herbal supplements like St. John’s Wort, all of which can increase serotonin levels in the brain. Symptoms of serotonin syndrome include agitation, confusion, rapid heart rate, and elevated blood pressure, and it can be potentially life-threatening if not treated promptly.
Moreover, because triptans can elevate blood pressure, they are contraindicated in patients with a history of hypertension or cardiovascular disease. Special caution should be exercised when prescribing these medications to patients with a history of stroke or heart disease.
Clinical Pharmacology Considerations
Triptans are classified as pregnancy category C in the United States, meaning their safety in pregnancy has not been established, and they should be avoided unless the potential benefit justifies the risk. Additionally, the pharmacokinetics of triptans vary between different agents. For instance, later-generation triptans tend to have longer half-lives and greater oral bioavailability compared to the older triptans like sumatriptan. This can lead to more convenient dosing regimens and a reduced likelihood of needing repeat doses.
Conclusion
Triptans have revolutionized the treatment of acute migraine and cluster headaches, providing rapid and effective relief for many patients. By targeting serotonin receptors in the brain, triptans help reduce vasodilation, inhibit pain transmission, and reduce the release of neuropeptides involved in headache pathophysiology. While generally well-tolerated, triptans do carry the risk of side effects, including cardiovascular events, and should be used with caution in certain populations. As our understanding of these medications continues to evolve, triptans remain a cornerstone of acute headache management.