|
Getting your Trinity Audio player ready... |
IMPURITIES IN NEW DRUG PRODUCTS Q3B (R2)
1. INTRODUCTION
1.1 Objective of the Guideline
IMPURITIES: This document aims to provide guidance to applicants seeking to register new drug products that have been produced using chemically synthesized new drug substances, which have not previously been registered within a given region or member state. The focus is on the content and qualification of impurities found within these drug products, helping to establish clear expectations and regulatory requirements for impurities that may arise during production.
1.2 Background: IMPURITIES
The guidelines set forth in this document are intended to complement the existing ICH Q3A(R) guideline, titled “Impurities in New Drug Substances.” For fundamental principles concerning the identification and control of impurities in new drug substances, the ICH Q3A(R) guideline should be consulted in detail. Additionally, for matters related to residual solvents, the ICH Q3C guideline on “Residual Solvents” should be referred to when applicable. Both guidelines provide essential frameworks that support the control and reporting of impurities within new drug substances and products.
1.3 Scope of the Guideline
This guideline specifically addresses impurities in new drug products that are classified as degradation products of the drug substance. These degradation products may result from chemical reactions involving the drug substance itself, excipients, or the immediate container closure system. These collectively are referred to as “degradation products” in this guideline. It is important to note that impurities found in the new drug substance do not need to be monitored in the drug product, unless they are also degradation products (refer to ICH Q6A on drug product specifications for further details).
Impurities originating from excipients in the drug product, as well as those leached or extracted from the container closure system, fall outside the scope of this guideline. Moreover, this guideline does not apply to drug products that are used during clinical research phases of development. Several product categories are explicitly excluded from the guidelines, including biological and biotechnological products, peptides, oligonucleotides, radiopharmaceuticals, fermentation products, semi-synthetic products derived from such sources, herbal products, and raw animal or plant-based products. Other exclusions encompass extraneous contaminants (which are typically addressed under good manufacturing practice or GMP regulations), polymorphic forms, and enantiomeric impurities.
2. RATIONALE FOR REPORTING AND CONTROL OF DEGRADATION PRODUCTS
Applicants are required to provide a comprehensive summary of the degradation products observed during the manufacturing process or in stability studies of the new drug product. This summary should be grounded in a sound scientific evaluation of the potential degradation pathways that the drug substance may undergo in the product, as well as impurities resulting from interactions with excipients or the container closure system.
The summary should also include details about laboratory studies conducted to identify degradation products within the new drug product. Such studies should span both batches produced during the development phase and those that represent the commercial production process. A thorough rationale should be provided for excluding impurities that do not qualify as degradation products, such as process impurities from the drug substance or impurities originating from excipients.
It is essential that the impurity profiles of the batches representing the proposed commercial process be compared with those from earlier development batches. Any differences between these profiles should be thoroughly explained.
If degradation products are detected during stability studies conducted under recommended storage conditions and are present above the identification threshold specified in Attachment 1, these products should be identified. If identification of a degradation product is not feasible, the applicant must provide a detailed summary of laboratory efforts that were made in trying to identify the product.
Degradation products present at concentrations below the identification threshold generally do not require identification. However, should a degradation product be suspected to have toxic or other significant pharmacological effects, even at levels below the threshold, analytical methods should be developed for its detection. In specific situations, where technical considerations such as manufacturing capabilities, excipient ratios, or the use of raw materials from plant or animal origins are involved, alternative thresholds may be proposed and justified based on the experience with the manufacturing process.
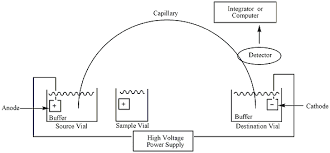
3. ANALYTICAL PROCEDURES
The registration application must include documented proof that the analytical procedures used to detect and quantify degradation products have been validated. These procedures should be in line with ICH Q2A and Q2B guidelines on analytical validation. Analytical methods must demonstrate specificity for the target degradation products, both identified and unidentified.
As part of the validation, analytical procedures should also include testing under relevant stress conditions—such as light exposure, elevated temperatures, humidity, acid/base hydrolysis, and oxidation—to ensure that they can accurately detect degradation products in a variety of conditions that might occur during production and storage.
When analytical methods reveal the presence of peaks other than those of the degradation products—such as peaks from the drug substance itself, impurities from the synthesis of the drug substance, excipient impurities, and impurities from excipients—these should be clearly labeled in the chromatograms. The origin of these peaks must be explained in the validation documentation.
The quantification limits for the analytical procedures must be set at or below the reporting threshold, as specified in the relevant guidelines. Degradation product levels can be determined using various techniques, including comparisons to reference standards or to the response of the new drug substance itself. Reference standards used in these procedures must be evaluated and characterized appropriately for their intended use. If the response factors between the degradation product and the drug substance differ significantly, appropriate correction factors must be applied to ensure accurate quantification.
It is also crucial that the registration application addresses any assumptions made in the analytical procedures, such as those based on equivalent detector response. Discrepancies between the analytical methods used during development and those proposed for commercial batches should also be discussed in detail.
4. REPORTING DEGRADATION PRODUCT CONTENT OF BATCHES
For every relevant batch of the new drug product, analytical results must be provided in the registration application. These should cover batches used for clinical, safety, and stability testing, as well as batches representative of the proposed commercial process. Quantitative results must be reported numerically and should not be generalized (e.g., stating “meets limit” or “complies” is insufficient).
Any degradation product found at a level above the reporting threshold (as outlined in Attachment 1) should be reported, along with the total degradation products observed across relevant batches. Results for degradation products should be reported with a level of precision appropriate to the magnitude of the concentration. For degradation products present at levels below 1.0%, results should be reported to at least two decimal places (e.g., 0.06%). For values at or above 1.0%, results should be reported to one decimal place (e.g., 1.3%).
It is highly recommended that results be tabulated in a spreadsheet format to provide clarity and structure. Each degradation product should be identified using a code or descriptor (such as retention time), with the appropriate analytical method used to detect it. In cases where a higher reporting threshold is proposed, it should be fully justified.
Chromatograms or equivalent data from representative batches, including long-term and accelerated stability studies, should be included in the application. If requested, complete degradation product profiles, including chromatograms, should be made available for individual batches. Each batch of the new drug product should include the following information in the registration documentation:
- Batch identity, strength, and size
- Manufacture date and location
- Manufacturing process
- Immediate container closure details
- Degradation product content (both individual and total)
- The intended use of the batch (e.g., clinical trials, stability testing)
- Reference to the analytical procedures used
- Batch number of the drug substance
- Storage conditions for stability studies
5. LISTING DEGRADATION PRODUCTS IN SPECIFICATIONS
The specification for a new drug product should clearly list the degradation products anticipated to form during manufacture and under recommended storage conditions. This list should be based on stability studies, knowledge of potential degradation pathways, and product development studies.
Degradation products that are included in the specification should be classified as “specified degradation products.” These can be either identified or unidentified. The decision to include a degradation product in the specification should be based on the degradation profiles observed during stability studies, safety evaluations, and clinical development phases, particularly for batches manufactured under the proposed commercial process.
The inclusion of specified degradation products in the specification should also consider whether the degradation products are toxic or have other pharmacological effects. In such cases, the detection and quantification limits of the analytical methods must be commensurate with the level at which these products need to be controlled.
For unidentified degradation products, the method used to estimate their level must be explicitly stated, along with any assumptions made. Additionally, an acceptance criterion of not more than the identification threshold should be applied for any unspecified degradation products, and total degradation products should also be included in the specification.
6. QUALIFICATION OF DEGRADATION PRODUCTS
Qualification involves gathering and evaluating data to ensure that individual degradation products, or specific degradation profiles, do not pose a risk to biological safety at the specified levels. Degradation products that have been tested in clinical or safety studies are generally considered qualified.
Qualification data should include details of the degradation product levels in the relevant batches used during clinical studies, as well as any available information on the safety of these products. If the degradation product levels exceed established thresholds and there is no existing qualification data, further studies may be required to establish safety.
In certain circumstances, a degradation product can be considered qualified based on previous safety and clinical study data, even if the levels in the new drug product are higher than those administered in earlier studies. Such instances must be justified based on clinical experience, drug class effects, and patient safety considerations